Monday, March 20, 2017
Thursday, February 9, 2017
FRCR 2B Rapid Reporting : CXR cases
The rapid reporting cases when we sometimes miss the finding include:
- Subtle pneumothorax (especially Apical and Supine PT).
- Apical pulmonary nodule / mass.
- Lytic lesion rib.
- Mastectomy.
Other less subtle ones include : Rib fracture, distal clavicular fracture, Left Upper Lobe collapse, Right middle lobe pneumonia, RLL/LLL collapse.
Patterns of pulmonary edema, SPN, Hilar lymphadenopathy, lobar consolidation are usually the obvious 'abnormal's in the exam, which should not pose any problems.
Ill-defined air-space opacification in right mid-zone, with poor definition of right cardiac margin (loss of silhouette), consistent with a right middle lobe pneumonia. Unless careful, can pass this as normal.
Case courtesy of Dr Jan Frank Gerstenmaier, Radiopaedia.org. From the case rID: 25805
The above case is a case of D10 ivory vertebra due to sclerotic metastasis from breast Ca.
However for the RR purpose, see the left mastectomy, with increased transradiancy of left hemithorax.
In addition there are few surgical clips seen in the lateral chest wall on left side.
The above image shows how to follow a checklist in each CXR case. The importance to follow a checklist for each region cannot be discounted in any case. This image also shows how subtle rib lytic lesions can be.
Click here for the Chest Radiograph RR Checklist
However for the RR purpose, see the left mastectomy, with increased transradiancy of left hemithorax.
In addition there are few surgical clips seen in the lateral chest wall on left side.
The above image shows how to follow a checklist in each CXR case. The importance to follow a checklist for each region cannot be discounted in any case. This image also shows how subtle rib lytic lesions can be.
Click here for the Chest Radiograph RR Checklist
Good web resources for RR:
2. Radiopaedia ( Now have 6 packets of RR free).
4. FRCR Academy (Paid Membership, ~30 RR packets).
5. Dr. Sameer Shamshuddin's Website : This site has numerous other resources and links for FRCR.
6. Dr. Gaurav Shankar's FRCR 2B Tips.
6. Dr. Gaurav Shankar's FRCR 2B Tips.
Xanthogranulomatous Cholecystitis (Histology from Imaging)
Male patient, 65 years, presenting with vague right hypochondrial pain. On USG showing marked diffuse thickening of gall bladder wall, measuring up to 20mm maximum thickness. Increased vascularity is also noted within the thickened GB wall.
GB lumen showed a large 20.5mm x 18.6mm calculus, with associated luminal sludge.
Above image showing marked thickening of GB wall on left and ill-defined interface of thickened GB wall with hepatic parenchyma (segment V).
A radiologist in his / her report if can suggest the histopathological diagnosis, I believe that would be an ideal situation. Its never easy even with history, clinical diagnosis, lab tests. The ill-defined margins of thickened GB wall and hepatic parenchyma, was suspicious of infiltration. CA-19-9 value was not available at the time of scan. CECT Abdomen was also performed without much significant added information. There were no significant lymphadenopathy / other focal liver lesions / ascites. Close differentials of XGC and Ca.GB were given. Patient underwent surgery, in which GB wall seen adherent to liver and a partial resection of involved parenchyma was also done. HPR came as Xanthogranulomatous Cholecystitis.
Tuesday, February 7, 2017
'Hummingbird and Morning Glory' of Radiology
Progressive Supranuclear Palsy (PSP) (Syn : Steele-Richardson-Olszewski Syndrome)
- Adult onset neurodegenerative disorder. Taupathy.
- Characterized by early postural instability leading to backward falls within the first year, abnormal eye movements due to supranuclear vertical gaze palsy and abnormal cognition.
- Important to distinguish PSP from Parkinsons Disease and and others like MSA as levodopa is less or no efficacious in treatment in PSP.
- PSP shows marked dorsal midbrain atrophy, with reduction in AP diameter.
- MRI describes few signs in Progressive Supranuclear Palsy namely the Hummingbird sign (aka Penguin Sign), Morning Glory Sign.
- Reduction in the ratio of areas of Midbrain and Pons is described in PSP.
- Other signs include widening of the Inter Peduncular Cistern and Reduced AP distance of the midbrain at the level of superior colliculus from the interpeduncular fossa to the intercollicular groove (<12mm).
- Increased T2 signal of midbrain and olives, atrophy and increased signal intensity of superior cerebellar peduncles are also seen.
- Bilateral putamina can show hypointense signal intensity due to increased iron content.
- Associated frontal and parietal atrophy are also seen. Third ventricle is usually dilated.
Above image shows the method of assessing for Morning Glory sign.
Again a normal patient with convex lateral margin of tegmentum.
Above image showing the concave lateral margin of tegmentum, termed as the Morning Glory Sign, which has been stated as a more specific sign of Progressive Supranuclear palsy.
Above images shows the comparison with a normal midbrain showing the superior convex contour and that of an atrophic midbrain showing concave superior contour in a Progressive Supranuclear Palsy patient. The appearance is likened to that of a Humming Bird.
Note : In the original article, the Morning glory sign, is described as the authors saw a likeness of atrophied midbrain to the lateral view of morning glory flower.
References :
1. Magn Reson Med Sci. 2004 Dec 15;3(3):125-32. Morning glory sign: a particular MR finding in progressive supranuclear palsy. Adachi M(1), Kawanami T, Ohshima H, Sugai Y, Hosoya T.
2. CT and MRI of the Whole Body, 6th Edition, John.R.Haaga, Elsevier Publications.
3. Humming bird and Morning glory images from pixabay.com , under CC0.
Saturday, January 28, 2017
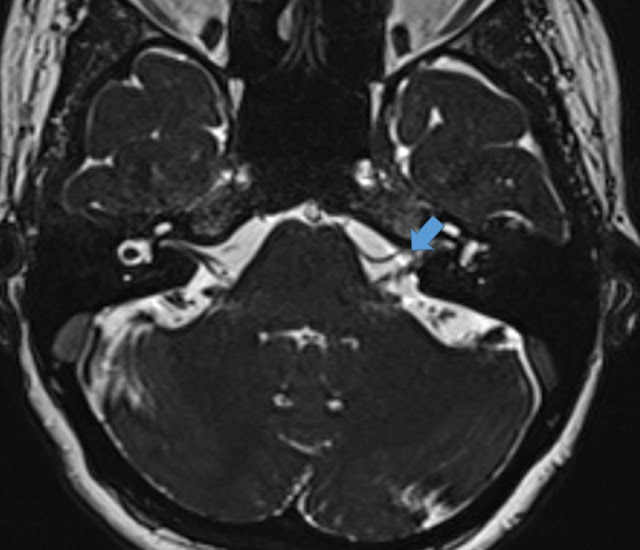
 What's 'GRE Susceptibility Vessel Sign' ?
What's 'GRE Susceptibility Vessel Sign' ?

Thrombi are mainly of three types based on their composition : platelet rich (white) thrombi, red thrombi containing rich fibrin network and RBCs and finally the mixed ones. White thrombi are formed mainly in atherosclerotic plaque ruptures, where as red thrombi are formed in low pressure systems like cardiac or venous systems.
The oxyhemoglobin which gets degraded into de-oxy hemoglobin, methemoglobin and hemosiderin, all have paramagnetic properties and produces susceptibility artifacts in GRE images. This concept is the main core of Susceptibility Vessel Sign.
Teaching Point : GRE SVS is associated with red thrombi and thereby favors a Cardio-Embolic Stroke in most cases. And it also signifies increased chance of subsequent spontaneous recanalization and also increased success rates with fibrinolytic therapy.
Exceptions :
1.SVS –ve cardio-embolic thrombi :
Can occur if MRI was taken before the degradation of Oxy-Hb to Deoxy-Hb (which usually occurs in few hours) OR due missing the section of small thrombus in GRE due to the interslice gap.2.SVS +ve (Large Artery) Atherosclerotic thrombi :
due to the formation of white thrombus initially, can lead to stagnant or reduced flow velocity within the vessel, there by gradually causing increased fibrin and RBC content of thrombus.References :
1. Significance of Susceptibility Vessel Sign on T2*-Weighted Gradient Echo Imaging for Identification of Stroke Subtypes. Kyung-Hee Cho, MD; Jong S. Kim, MD, PhD; Sun U. Kwon, MD, PhD; A-Hyun Cho, MD; Dong-Wha Kang, MD, PhD. Stroke, November 2005.
Wednesday, January 25, 2017
Monday, January 23, 2017
Calculus in Wharton's Duct in a post submandibular sialadenectomy patient !!
Female patient post sub-mandibular sialadenectomy for calculous sialadenitis. Now complaining of a sublingual hard swelling (at the site of opening of Wharton's Duct).
Above USG image is obtained from the right submandibular region,
along the length of the Wharton's duct, with shows a terminal calculus,
measuring ~8.5mm x 4.0mm, with duct measuring upto 3.9mm proximally.
Axial view from the neck, showing the calculus at the opening of right submandibular duct.
Chronic Pelvi-Ureteric Junction Obstruction (PUJO)
1 yr old child on follow-up for prenatally detected renal pelvic dilatation.
Marked renal pelvic dilatation is noted with gross hydronephrosis. The renal pelvis appeared 'ballooned' and the dilatation appears to be disproportionate to the degree of calyceal dilatation.
The AP diameter of renal pelvis measures 39mm (3.9cm). The dilated pelvi-calyceal system is showing internal echogenic particles. There is no past history of UTI.
High resolution USG with the linear 12MHz probe showed better the
marked thinning of renal parenchyma, measuring ~2mm only.
marked thinning of renal parenchyma, measuring ~2mm only.
View of the ballooned markedly dilated renal pelvis with the linear probe.
Saturday, January 21, 2017
Aggressive ('Malignant') Hemangioma of Vertebrae
Vertebral hemangioma is a benign vascular tumor, usually affecting the vertebral body.
The typical benign (ones with fatty stroma) shows T1 and T2 hyperintense signal in MRI. In CT these show the pathognomonic 'Polka dot' appearance and 'corduroy' / 'jail house stripe' appearance in axial and coronal/sagittal sections.
The aggressive ('malignant') hemangiomas are T1 isointense to hypointense and T2 hyperintense with intense post-contrast enhancement. Pathologic fractures and epidural extension are common with aggressive hemangiomas. Cord compression can occur in the presence of epidural extension.
Aggressive Hemangioma features :
Location common in D3 to D9 vertebrae, with extension into posterior elements, expansion, indistinct cortex, irregular honeycomb pattern and associated soft tissue mass.Differential considerations in Aggressive Hemangioma include :
1. Metastases : Can be difficult, Correlative CT sections will be helpful.2. Paget's Disease : Can also present with vertebral body expansion, but will not have soft tissue component.
T2 WI Sagittal image showing hyperintense lesion of L3 vertebra, with vertebral body expansion and soft tissue component. Marked spinal canal stenosis with cauda equina compression seen.
Unlike simple hemangioma with predominantly fatty stroma, which gets suppressed in STIR images, aggressive hemangiomas consists of more vascular tissue and usually remains hyperintense in STIR.
.
T1 WI Sagittal and Axial Images, showing heterogeneous reduced signal intensity.
Intense enhancement in the post contrast images.
(1)Post contrast T1 FS Axial image. (2&3) correlative CT sections
showing the irregular honeycomb appearance and indistinct cortex.
References :
1. Diagnostic Imaging - Spine (Jeffrey.R.Ross), Ist Edition, 2004.
Tuesday, January 17, 2017
Intracranial Arachnoid Cyst : Galassi Type I
By definition an ARACHNOID CYST is an intra-arachnoid CSF-filled sac
that does not communicate with the ventricular system. Best diagnostic
clue is a sharply demarcated, round/ovoid extra-axial cyst that follows
CSF density/signal and shows no diffusion restriction or enhancement.
As its an extra-axial lesion it does buckles the grey-white interface and may also remodel / cause scalloping / thin adjacent bone.
It comprises of ~1% of all intracanial masses. Majority (~60%) are located in the middle cranial fossa, anterior the the temporal lobe, with posterior displacement of MCA. Less common sites of arachnoid cysts include CP angle, Suprasellar region, convexity and quadrigeminal cistern.
The major differential diagnosis will be an epidermoid cyst, porencephalic cyst, neurenteric cyst and neuroglial cysts. DWI and T2 FLAIR sequences are the most helpful in arriving at a diagnosis.
Epidermoid cysts show diffusion restriction. These lesions are only partially suppressed in T2 FLAIR images and looks 'dirty'. These are plastic lesions, which instead of displacing vessels engulf them and insinuate into the sulcal spaces.
A porencephalic cyst will usually have history of previous trauma or infarct. And these are usually surrounded by gliotic areas, not displaced cortex.
Neuroglial cysts are usually intra-axial.
Neurenteric cysts are usually seen in posterior fossa and they often contain proteinaceous fluid.
The following images depict the typical imaging findings of a middle cranial fossa arachnoid cyst.
In the anterior temporal location, it may be associated with temporal lobe hypoplasia. Above image shows complete homogenous supression of the signal of the arachnoid cyst in T2 FLAIR images.
Galassi et al. had classified middle cranial fossa arachnoid cysts into 3 types long back in 1982, this classification is still being followed.
Type I cyst : Located in the Sylvian fissure, in the anterior temporal region, posterior to the sphenoid ridge, without any mass effect. These freely communicate with the subarachnoid space in Contrast CT cisternogram or in Phase Contrast MR evaluation.
Type II cyst : Located in the mid and proximal portions of Sylvian fissure, larger and rectangular in configuration. They communicate with subarachnoid space but slowly.
Type III cyst : Usually do not communicate with subarachnoid cyst, largest, lentiform in shape, will result in signficant mass effect and midline shift.
NOTE : A very large arachnoid cyst can show T2 slightly hypointense signal due to internal flow.
As its an extra-axial lesion it does buckles the grey-white interface and may also remodel / cause scalloping / thin adjacent bone.
It comprises of ~1% of all intracanial masses. Majority (~60%) are located in the middle cranial fossa, anterior the the temporal lobe, with posterior displacement of MCA. Less common sites of arachnoid cysts include CP angle, Suprasellar region, convexity and quadrigeminal cistern.
The major differential diagnosis will be an epidermoid cyst, porencephalic cyst, neurenteric cyst and neuroglial cysts. DWI and T2 FLAIR sequences are the most helpful in arriving at a diagnosis.
Epidermoid cysts show diffusion restriction. These lesions are only partially suppressed in T2 FLAIR images and looks 'dirty'. These are plastic lesions, which instead of displacing vessels engulf them and insinuate into the sulcal spaces.
A porencephalic cyst will usually have history of previous trauma or infarct. And these are usually surrounded by gliotic areas, not displaced cortex.
Neuroglial cysts are usually intra-axial.
Neurenteric cysts are usually seen in posterior fossa and they often contain proteinaceous fluid.
The following images depict the typical imaging findings of a middle cranial fossa arachnoid cyst.
In the anterior temporal location, it may be associated with temporal lobe hypoplasia. Above image shows complete homogenous supression of the signal of the arachnoid cyst in T2 FLAIR images.
Above image shows the lesion being isointense to CSF in T1 WI.
In DWI-ADC, contrast from an epidermoid cyst, the arachnoid cyst shows no diffusion restriction.
Galassi et al. had classified middle cranial fossa arachnoid cysts into 3 types long back in 1982, this classification is still being followed.
Type I cyst : Located in the Sylvian fissure, in the anterior temporal region, posterior to the sphenoid ridge, without any mass effect. These freely communicate with the subarachnoid space in Contrast CT cisternogram or in Phase Contrast MR evaluation.
Type II cyst : Located in the mid and proximal portions of Sylvian fissure, larger and rectangular in configuration. They communicate with subarachnoid space but slowly.
Type III cyst : Usually do not communicate with subarachnoid cyst, largest, lentiform in shape, will result in signficant mass effect and midline shift.
NOTE : A very large arachnoid cyst can show T2 slightly hypointense signal due to internal flow.
Wednesday, January 4, 2017
Tuesday, December 20, 2016
Subscribe to:
Posts (Atom)

















 What's 'GRE Susceptibility Vessel Sign' ?
What's 'GRE Susceptibility Vessel Sign' ? What's your Diagnosis? : Question 1
What's your Diagnosis? : Question 1






























 Question 3 : Diagnosis?
Question 3 : Diagnosis?
